Enderby has suffered a tragic toll in B.C.'s ongoing toxic drug crisis.
Since 2016, the North Okanagan community has seen 19 people die from overdoses – eight of those in 2021 alone.
That grisly statistic puts Enderby at the third-highest rate of drug toxicity deaths in B.C.
On Monday, Interior Health, Splatsin First Nation, and the First Nations Health Authority held an awareness event at the Splatsin Community Centre.
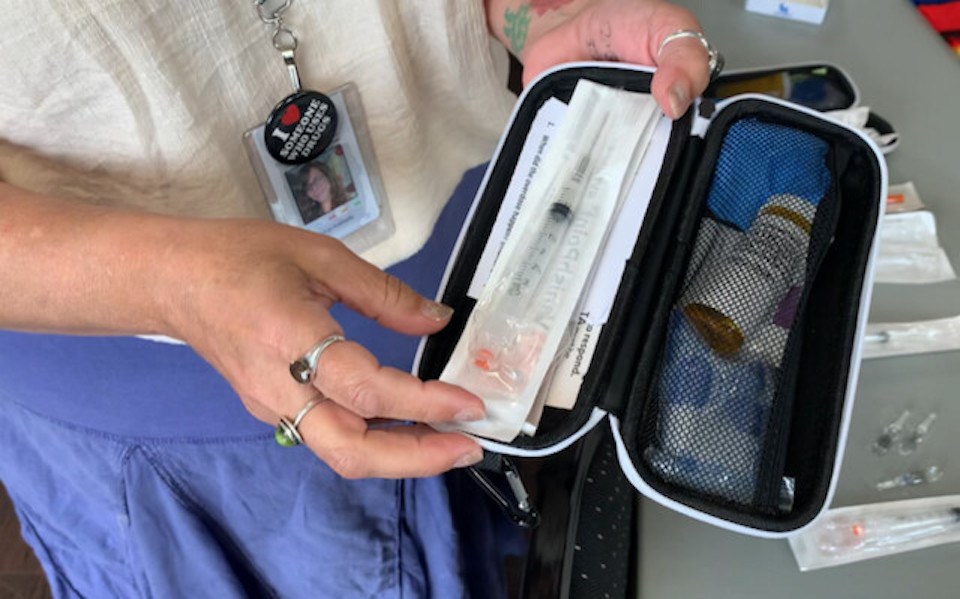
Community leaders learned about the local impact of the drug crisis and participated in hands-on Naloxone training, which can reverse the effects of an opioid overdose.
Harm-reduction educator Tonya Robitaille said: "It's always better to never need a Naloxone kit than to not have one when you do."
She said it's impossible to know how many people have been saved by Naloxone injections or nasal spray because authorities can't know how many of the kits get used. But, as a guide, she said she had handed out 500 kits in just the last month across the Interior Health region.
And she noted, if in doubt if a person is overdosing, it will do no harm to give them Naloxone anyway.
She said because of the growing toxicity of street drugs, it can take six, seven or even eight doses to revive a drug user who has fallen unconscious. In one recent instance, 11 shots had to be given.
The reason for this is the growing frequency with which powerful benzodiazepines are being cut into street drugs along with fentanyl.
Robitaille suggested giving a shot every five minutes until the person comes to, and rescue breaths every five seconds.
Kukpi7 (Chief) Doug Thomas said battling the crisis is not just a matter of erasing the stigma around drug use, but also one of prejudice and reconciliation.
"Just like any other prejudice, people pre-judge when it comes to drugs and alcohol," said Thomas. "It's one of the symptoms people must understand when it comes to truth and reconciliation.
"If you see someone on the street, you are only scratching the surface – you don't know what that person has been through."
Thomas says "there has definitely been a shift" in attitudes since the discovery of hundreds of children's graves at the former Kamloops Residential School made national headlines.
"People are starting to listen, not just with their ears, but with their hearts," he said.
"It still shocks me that there are some people who don't get it," he said in reference to the inter-generational trauma inflicted on First Nations families by the residential school system. "The Government of Canada had the impression we were savages as late as the 1950s.
"The bottom line is that every child matters ... so many over medicated themselves, so many died without realizing that their lives mattered."
Regional harm-reduction co-ordinator Alison Houweling said Naloxone kits are available from health units, pharmacies and at the Splatsin health centre.
OD prevention sites are located in Vernon, Kelowna, Kamloops, and there is a volunteer-run mobile clinic in Penticton, along with several private safe sites at BC Housing locations.
Robitaille said there has never been an OD death at a prevention site, and also urged the use of apps such as Lifeguard and BeSafe, which will dispatch help if a drug user does not respond to a text message.
Toxic drugs are the number 1 cause of death among 18-39 year olds in B.C. and the No. 2 cause of death for those 40-59.
Meanwhile, First Nations people are dying at 4.8 times the rate of the rest of the population.